Introduction
Physical therapy in Pittsburgh for Muscle Strains
Welcome to Greater Pittsburgh Physical Therapy & Sports Medicine’s resource on Muscle Strains.
Muscles make up over half of the weight of a human body and they are required to make even the smallest of movements such as nodding your head or tapping your toe. If too much stretch is put through one of your muscles you may end up with a painful muscle strain. If the similar type of injury occurred to one of the ligaments in your body, it is termed a sprain.

This guide will help you understand:
- the anatomy of a muscle
- what a muscle strain is and why it occurs
- how muscle strains are classified
- the symptoms of a muscle strain
- how your health care professional diagnoses a muscle strain
- what Greater Pittsburgh Physical Therapy & Sports Medicine’s approach to rehabilitation is
Anatomy
What parts of the body are involved?
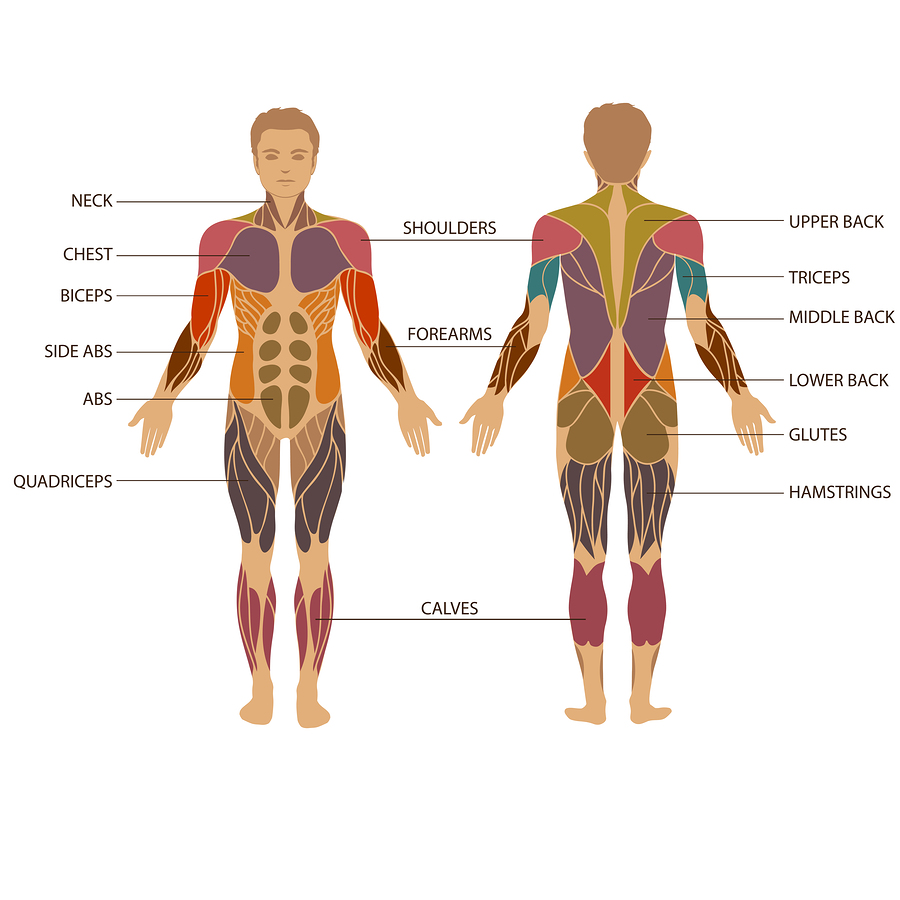
Muscles are composed of many fibers bundled together; the bigger, more frequently used muscles have more fibers than the smaller, lesser-used ones. Among the muscles are voluntary and involuntary muscles. Voluntary, or striated muscles, are those that we move by choice (for example, the muscles in your arms and legs). Involuntary muscles, or smooth muscles, are the ones that move on their own (for example, the muscles that control your diaphragm and help you breathe). The muscles in your heart are called involuntary cardiac muscles.
Voluntary muscles are attached to bones by tendons, a sinewy type of tissue. The area where the muscle attaches to the tendon is called the musculotendinous junction.
Causes
What causes a muscle strain?
A muscle strain, or a muscle pull occurs when a muscle in your body is overstretched or overworked. Even if the injury from overstretching or overworking occurs more to the attaching tendon it can also be classified under the term muscle strain. A muscle strain can occur in any of your voluntary muscles (or tendons which attach to the muscle), but they are most common in the low back, the calves, the front and back of the thighs, the pectoral muscles, and the muscles of the neck and the shoulder. Muscle strains occur more often in muscles that cross two joints (such as the thigh or calf muscles) and often occur when the muscles are working eccentrically (working while under a stretch). Most often a strain occurs at the musculotendinous junction but can occur anywhere along the muscle.
A muscle strain can occur due to a one-time overstretching or overworking of a muscle (acute injury) or can occur from repetitive use of a muscle over time (overuse injury).
Classification
How are muscle strains classified?
There are several classification systems developed and in use regarding muscle strains but the most commonly used system includes three grades. All muscle strains include tearing of some muscle fibers:
Grade I (mild): Very few muscle fibers have been injured. Pain may not be felt until the following day after the instigating activity. Strength and range of motion of the muscle remains full but pain can be felt when engaging the muscle often when it is at its end range of stretching. No swelling or bruising is noted.
Grade II (moderate): A large category including all strains between a grade I and grade III. Being that this category is so large, it is sometimes further divided into having a mild, moderate or severe grade II strain. With this category many muscle fibers are torn which results in a decrease in strength and often a limited range of motion. Some muscle fibers remain uninjured and intact. Pain is present both when stretching the muscle and on muscle strength testing. Swelling and bruising may be noted.
Grade III (severe): All fibers of the muscle are completely torn. This means that the muscle is completely torn into two parts or the muscle belly has torn from its attachment to the tendon. Severe swelling, pain, and bruising accompany a grade III strain. There is generally limited ability to generate any force on strength testing of the muscle due to the tear (however other muscles may compensate to initiate some strength) and the range of motion is either severely limited due to pain, or the range of motion testing may show excessive range due to the torn muscle not providing any limitation as it is stretched.
Symptoms
What does a muscle strain feel like?
Several symptoms can indicate that you have incurred a muscle strain but the symptoms you feel will depend on the grade of strain you have incurred:
- sudden onset of pain, or pain/soreness that comes on the next day related to a specific event
- pain on touching the injured area
- mild, moderate, or severely limited range of movement, or an extreme abnormal range of motion
- decreased strength in the injured muscle
- bruising or discoloration in the area or at a distal location to the strain
- swelling
- a "knotted up" feeling
- a local divot or bump in the affected area due to the torn muscle fibers
- muscle spasm in the area
- stiffness in the area

Diagnosis
How do health care professionals diagnose the problem?
Your physical therapist at Greater Pittsburgh Physical Therapy & Sports Medicine will ask a number of questions to determine if you have strained your muscle and to determine how severe the damage is. They will want to know exactly when you injured yourself and if you injured the muscle from one specific event or if a repetitive injury caused your pain. They will want to know what you felt immediately after the injury and whether or not you feel that you have lost any strength or range of motion. Your therapist will also want to know if there has been any swelling or bruising around the area or anywhere down one of your limbs. They will also want to know what sort of things are aggravating your pain or if you have been able to do anything to make your pain feel better. They will inquire about any medications you are taking and whether or not you have ever injured this muscle in the past.
After a thorough history your physical therapist will do a physical examination. Firstly they will observe how you are holding your affected limb or your neck or back, if this is the area in question. Next they will examine the area to determine if there is any swelling or bruising present. They will palpate (feel) your muscle to find out which area is most sore. They will also check to see if there are any divots or unusual bumps in the area, which would be the result of a section of torn muscle fibers; this would indicate a more severe strain. Finally, they will ask you to move your muscle in order to determine how much you can move it and whether or not moving it causes you pain. In order to help determine the severity of the strain your physical therapist will also assess how much they can passively stretch your injured muscle, and will check how much strength against resistance you can generate with your muscle. If you are able to they may ask you to push, pull, bend, stand, sit, or jump in order to help assess your strain. Lastly, they will check the integrity of the joints that are closest to your injured muscle to ensure that you haven’t also injured them.
After a thorough history and physical examination your physical therapist will determine the grade of your muscle strain. If they determine that your strain is severe (severe grade II or a grade III) they may send you to your physician for a review as further investigations are possibly required, and medication may be needed to control some of your symptoms. If you have a severe strain to one of your lower extremity muscles you may require the use of crutches in order to get around; your physical therapist can teach you how to use them. The general rule regarding when to use crutches is such that if you are limping when walking without crutches you should use crutches until your strain heals enough so that you are able to walk without limping when not using crutches.
Physician Review
What will my doctor do when I see them?
In the case of a severe strain (severe grade II or a grade III), a physician’s review may be necessary. When you see your physician, they may prescribe anti-inflammatory or pain medications to help control the swelling and assist with the pain.
Your physician will determine if a diagnostic investigation is required to further assess your muscle strain. In most cases an X-ray is not necessary unless your physician is concerned that you may have also fractured the bone, in which they will order an X-ray to rule this out. Diagnostic ultrasound is a timely way to image muscle groups to determine strain severity. In cases of severe strains, a magnetic imaging resonance (MRI) test may be ordered to confirm the muscle that has been injured, and to determine the exact amount of damage to the muscle, particularly if it looks severe enough to warrant surgical consideration. An MRI has the benefit of confirming the exact severity of the muscle strain. Grade I or grade II strains that are mild to moderate do not generally require any investigative reviews but may benefit from the use of pain or anti-inflammatory medications.
Rehabilitation
The initial approach to physical therapy of your muscle strain will depend on how long after your injury that you seek treatment. The immediate line of defense straight after a muscle strain should be the application of ice and compression, followed by rest and elevation for the affected muscle. Recent research on the benefits of applying ice immediately after an injury are beginning to be questioned, but the general consensus is still to apply ice. The importance of applying compression initially as a line of first defense (generally done by wrapping the affected area) is becoming more evident.
The initial aim of treatment for acute strains at Greater Pittsburgh Physical Therapy & Sports Medicine is to manage the inflammation and pain in the area. The initial aim of treatment for acute muscle strains at Greater Pittsburgh Physical Therapy & Sports Medicine is to decrease the pain as well as any secondary inflammation in the area. Some initial inflammation is actually required to start the healing process, but a large inflammatory response can also lead to secondary inflammation and secondary cell injury, which affects tissues that were not directly related to the initial insult. Ice and compression can greatly assist in decreasing this detrimental secondary tissue injury.
In cases where it is not an acute strain heat may be more useful in decreasing pain. Your physical therapist can advise you whether it is best to use ice or heat at your stage of healing. Your therapist may also use electrical modalities such as ultrasound or interferential current to help decrease the pain and control the amount of inflammation. It should be noted, however, that some mild inflammation is actually needed in order for the muscle to heal; all anti-inflammatory attempts are aimed at controlling too much inflammation from occurring, rather than completely eliminating it. Massage of the injured area or the tissues surrounding the area may also be helpful. Depending on the severity of the strain and the time that has elapsed since the injury, massage directly over the torn area can slow the healing process and may lead to other muscle complications so be sure to let your physical therapist determine whether or not this is something you should be doing on your own.
As indicated above, medication to ease the pain or inflammation can often be very beneficial in the overall treatment of a muscle strain. Depending on the degree of your strain your physical therapist may suggest you see your doctor to discuss the use of anti-inflammatories or pain-relieving medications in conjunction with your physical therapy treatment. Your physical therapist may even liaise directly with your doctor to obtain their advice on the use of medication in your individual case.
Once the initial pain and inflammation has calmed down, your physical therapist will focus on improving the flexibility and strength of the involved muscle. Static stretches to increase the flexibility of the muscle will be prescribed by your physical therapist early on in your treatment as these types of stretches encourage the healing tissues to withstand stretch and they ensure that you do not lose any range of motion overall. As your range of motion improves, more aggressive stretches will be added, however stretching should be limited such that it never causes pain. Feeling a gentle stretch at the end of the range of motion should be the limit otherwise further damage could occur to the muscle. As the muscle nears the end of its healing, dynamic stretching (rapid motions that stretch the tissues quickly) will also be taught and will be incorporated into your rehabilitation exercise routine in order to prepare your muscle to return to more taxing movements such as those involved in normal everyday activity or sport. Dynamic stretches are used to prepare the tissues for activity whereas static stretches focus more on gaining flexibility.
Rest is also an important part of your physical therapy treatment. ‘Relative rest’ is a term used to describe a scale of resting compared to the normal activity you would be doing. If you are experiencing pain while doing nothing at all it means the injury is more severe and your physical therapist may advise a period of complete rest where you do either no activity, or very little activity such as a few gentle stretches. As your pain improves then the rest to activity balance will swing the other way such that you will still require more rest for the muscle than usual but there will also be a gradual increase in activity including more aggressive stretches along with strengthening so long as there is no return in symptoms.
Along with stretching exercises, your physical therapist will also prescribe strengthening exercises in order to get your strained muscle back in top shape. Initially your therapist may suggest that you only do isometric contractions of your muscle, which means that you tighten the affected muscle without actually moving the associated joints. An example of this type of contraction occurs when people are asked to flex their biceps muscle, and they tighten the muscle fibers of the upper arm in place, without bending the elbow or moving the shoulder. This type of contraction is an effective way to begin strengthening an injured muscle. As the muscle continues to heal, more aggressive strengthening will be prescribed where you are moving your limb and using the weight of your body to provide resistance. When appropriate your therapist will prescribe strengthening exercises with free weights, elastic bands or tubing, weight machines, or cardiovascular machines such as stationary bicycles or a treadmill in order to continue to increase the strength and endurance in your injured muscle. As your strained muscle is more fully healed, your therapist will add eccentric type strengthening to your rehabilitation program. Eccentric exercises are ones that put load through your muscle as it is lengthening.
These types of exercises are necessary as part of your rehabilitation program in order to prepare the strained muscle for the return to normal everyday activity and sport. Quite often it is an eccentric contraction of the muscle that has caused the strain in the first place, so training the muscle to withstand this type of force when the time is right is crucial to ensuring it won’t be re-injured.
In addition to stretching and strengthening the muscle, taping or wrapping the affected muscle with an elastic bandage may be done by your physical therapist in order to assist initial swelling, and to provide support to the muscle as you rehabilitate it. They may even teach you how to tape or wrap your own muscle so you can do it on your own.
If your muscle strain is in the lower part of your body, your therapist may prescribe a specific type of strengthening called plyometrics. Plyometrics is a form of power strengthening that is a particularly important part of the end stage of your rehabilitation for any of your power muscles in your legs such as your quads, hamstrings, and calves, especially if you are involved in sport. Plyometrics involves repetitive jumping which forces your muscles to engage in force as they repetitively shorten and lengthen. This type of training maximally loads the lower extremity muscles and prepares them to take the high stress load involved with activity such as sport or daily activities such as running across the street.
A critical part of our treatment for a muscle strain at Greater Pittsburgh Physical Therapy & Sports Medicine includes advice on finally returning to your normal physical activity level. Strained muscles can easily be aggravated if too much stress is put through them at an inappropriate time. Returning to your normal physical activity at a graduated pace is crucial to avoiding repetitive muscle strains of the same muscle or a chronic injury. Advice from your physical therapist on the acceptable level of activity at each stage of your rehabilitation process will be invaluable, and will assist you in returning to your activities as quickly but as safely as possible.
*New research is emerging examining the use of ice in acute injury and suggests that ice may slow down the inflammatory response necessary to initiate healing. As the body of literature grows and practice changes we will be sure to update our recommendations.
Complications
What kinds of complications can occur from a muscle strain?
The healing of a muscle strain may result in a complication, which is more common when dealing with a severe than mild strain. Factors that may affect the risk of developing a complication include stretching the muscle too aggressively and too early on, not having an appropriate time to heal before returning to activity, or massaging directly over the strain too aggressively.
The most common complication with a muscle strain is a re-injury which most often results from returning to activity too soon before the tear is healed. In order to ensure you don’t do too much too soon, strictly follow the advice of your physical therapist in regards to your stretching, strengthening, and return to everyday and sporting activity.
In more severe strains, hematomas (blood clots) can develop as a complication within the healing muscle. The hematoma is felt as a hard lump in the muscle fairly early on in the recovery process. The development of a hematoma can delay recovery time, but the hematoma, in most cases, will eventually be reabsorbed back into the tissue, and a full recovery will be made.
In some cases of muscle strains myositis ossificans (MO) may develop. This condition occurs most commonly in strains of the quadriceps muscle but can occur in any strained muscle. In this condition damaged muscle fibers turn into small bone fragments (ossify) but the exact mechanism of this conversion remains unclear. MO will also cause a lump in the healing tissue, similar to a hematoma, but the calcification of the muscle will not be felt or show up on X-ray usually any earlier than approximately 4 weeks after the injury, which distinguishes it from a hematoma. Being too aggressive in early rehabilitation or returning to activity too early may be related to developing MO. See Greater Pittsburgh Physical Therapy & Sports Medicine’s Guide to Myositis Ossificans.
Another complication of severe muscle strains can be a compartment syndrome. When a severe strain occurs there is a lot of local swelling and blood in the area, which has nowhere to escape to. The force of the extra fluid in the area can put pressure on the other local muscles and arteries and can cause severe damage or death to the muscles by cutting off their blood supply. Symptoms of a compartment syndrome can include a sudden, new and excessive pain or ache in the injured area, pins and needles or tingling, difficulty moving the body part, and tightness on palpation of the area. An acute compartment syndrome requires immediate medical attention in order to decompress the compartment, restore blood supply to the tissues, and ensure no muscle death occurs in the affected area.
A severe muscle strain may also result in a much less common, but serious, complication call rhabdomyolysis. In this condition muscle fibers rapidly die off and muscle protein and enzymes are then released into the blood stream and out in the urine. Due to the muscle protein and enzymes traveling in the blood stream, rhabdomyolysis can cause symptoms related to not just the local muscle, but also the entire functioning of the body including kidney problems. The condition of rhabdomyolysis can also be caused by other injuries than a muscle strain. Rhabdomyolysis may be difficult to diagnose but can cause symptoms such as ongoing muscle pain, weakness and stiffness, as well as darkened urine. Rhabdomyolysis itself can be the cause of a compartment syndrome in the area. If rhabdomyolysis is suspected, a blood and urine test will be required to confirm the diagnosis. Treatment of rhabdomyolysis can be complicated and will depend on the severity of the condition as well as the initial cause of it.
Conclusion
Muscle strains involve a tear to the fibers of a muscle and vary in healing time depending on how severe the strain is. If you experience a muscle strain, let the expert physical therapists at Greater Pittsburgh Physical Therapy & Sports Medicine assist you in determining the severity of your strain as well as help get you back to your everyday activity or sport by guiding you through the appropriate rehabilitation program.
