Introduction
Physical therapy in Pittsburgh for Whiplash
Welcome to Greater Pittsburgh Physical Therapy & Sports Medicine's patient resource about Whiplash.
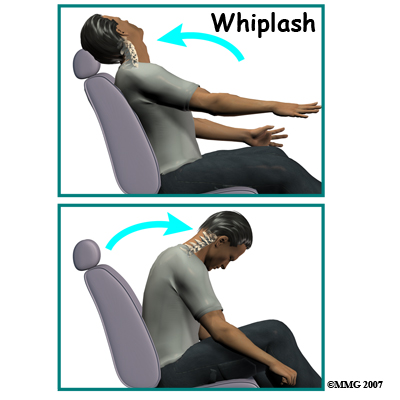
Whiplash is defined as a sudden extension (backward movement of the neck) and flexion (forward movement of the neck) of the cervical spine. This type of trauma is also referred to as a cervical acceleration-deceleration (CAD) injury. Rear-end or side-impact motor vehicle collisions are the number one cause of whiplash with injury to the muscles, ligaments, tendons, joints, and discs of the cervical spine.
This guide will help you understand:
- what parts make up the spine and neck
- what causes this condition
- how doctors diagnose this condition
- what treatment options are available
Anatomy
What parts of the spine are involved?
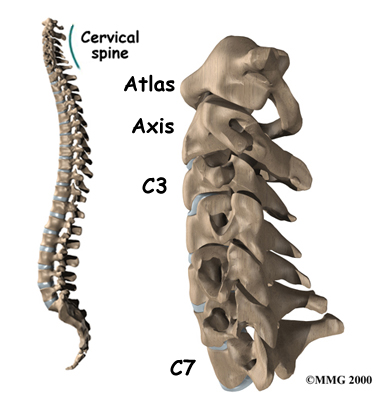
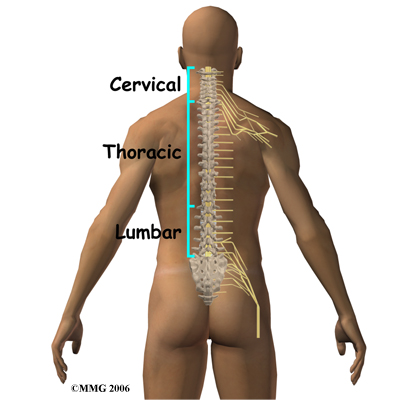
The human spine is made up of 24 spinal bones, called vertebrae. Vertebrae are stacked on top of one another to form the spinal column. The spinal column is the body's main upright support.
The cervical spine is formed by the first seven vertebrae referred to as C1 to C7. The cervical spine starts where the top vertebra (C1) connects to the bottom edge of the skull. The cervical spine curves slightly inward and ends where C7 joins the top of the thoracic spine. This is where the chest begins.
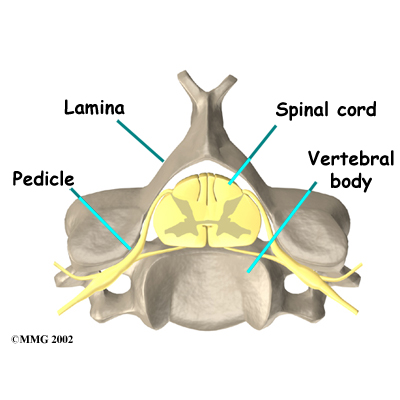
A bony ring attaches to the back of the vertebral body. When the vertebrae are stacked on top of each other, the rings form a hollow tube. This bony tube surrounds the spinal cord as it passes through the spine. Just as the skull protects the brain, the bones of the spinal column protect the spinal cord.
As the spinal cord travels from the brain down through the spine, it sends out nerve branches between each vertebrae called nerve roots. The nerve roots that come out of the cervical spine form the nerves that go to the arms and hands.
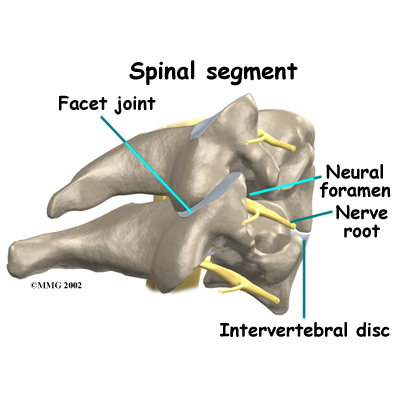
Two spinal nerves exit the sides of each spinal segment, one on the left and one on the right. As the nerves leave the spinal cord, they pass through a small bony tunnel on each side of the vertebra, called a neural foramen. (The term used to describe more than one opening is neural foramina.)
Each spinal segment includes two vertebrae separated by an intervertebral disc, the nerves that leave the spinal cord at that level, and the small facet joints that link each level of the spinal column.
An intervertebral disc is made of connective tissue. Connective tissue is the material that holds the living cells of the body together. The disc is a specialized connective tissue structure that separates the two vertebral bodies of the spinal segment. The disc normally works like a shock absorber. It protects the spine against the daily pull of gravity. It also protects the spine during activities that put strong force on the spine, such as jumping, running, and lifting.
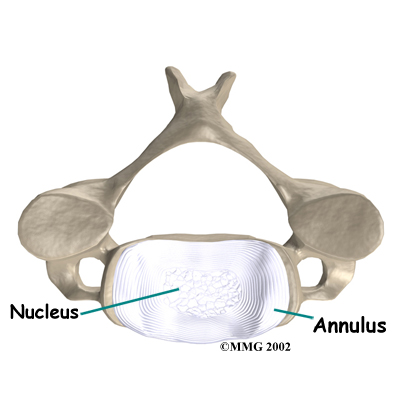
An intervertebral disc is made up of two parts. The center, called the nucleus, is spongy. It provides most of the ability to absorb shock. The nucleus is held in place by the annulus, a series of strong ligament rings surrounding it. Ligaments are strong connective tissues that attach bones to other bones.
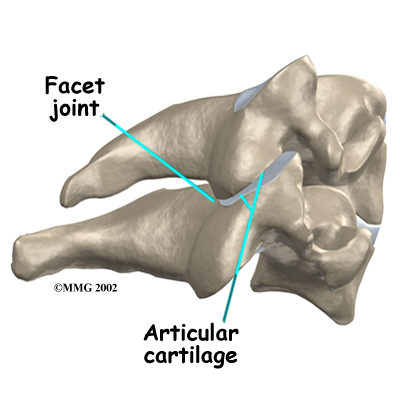
There are two facet joints between each pair of vertebrae--one on each side of the spine. The surfaces of the facet joints are covered by articular cartilage. Articular cartilage is a smooth, rubbery material that covers the ends of most joints. It allows the bone ends to move against each other smoothly, without pain. The alignment of the facet joints of the cervical spine allows freedom of movement as you bend and turn your neck.
Related Document: Greater Pittsburgh Physical Therapy & Sports Medicine's Guide to Cervical Spine Anatomy
Causes
What causes this condition?
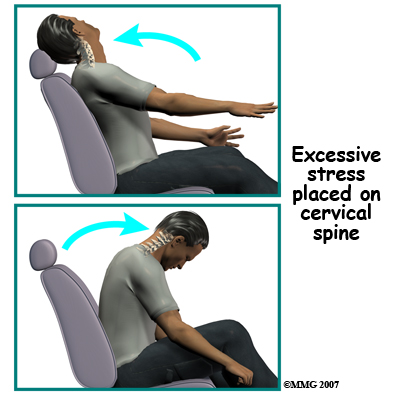
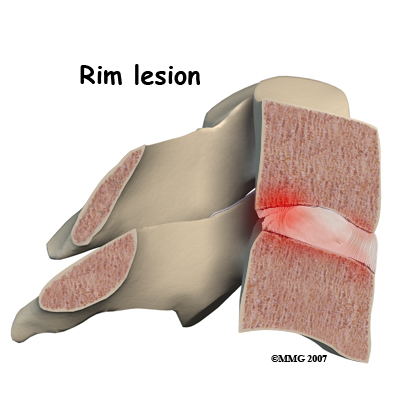
When the head and neck are suddenly and forcefully whipped forward and back, mechanical forces place excessive stress on the cervical spine. Traumatic disc rupture and soft tissue damage can occur. The cartilage between the disc and the vertebral bone is often cracked. This is known as a rim lesion.
Damage to the disc can put pressure on the nerves as they exit the spine. The pressure or irritation can be felt as numbness on the skin, weakness in the muscles, or pain along the path of the nerve. Most people think of these symptoms as indications of a pinched nerve. Health care providers call this condition cervical radiculopathy.
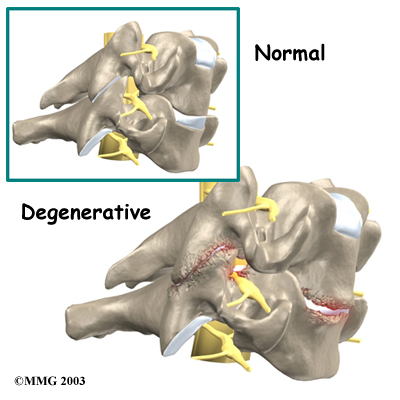
Soft tissue around the facet joint can be injured. Many of the pain-sensing nerves of the spine are in the facet joints. The normally smooth surfaces on which these joints glide can become rough, irritated, and inflamed. Studies show that neck pain often comes from the damaged facet joints.
Low back pain is a common feature after a whiplash injury. Studies show that there is significant electrical activity in the muscles of the lumbar spine when the neck is extended. This effect increases when there is neck pain, possibly as a way to help stabilize the spine when neck pain causes weakness.
More than anyplace else in the body, the muscles of the neck sense sudden changes in tension and respond quickly. Tiny spindles in the muscles signal the need for more muscle tension to hold against the sudden shift in position.
The result is often muscle spasm as a self-protective measure. The increased muscle tone prevents motion of the inflamed joint. You may experience neck stiffness as a result.
Risk Factors
Each year, about three million people experience whiplash injuries to their neck and back. Of these three million people, only about one-half, will fully recover. About 600,000 of those individuals will have long-term symptoms, and 150,000 will actually become disabled as a result of the injury.
There are many factors that come into play when a person is injured in a rear-end motor vehicle accident. Any one or more of the following factors can affect recovery:
- Head turned one way or the other at the time of the impact (increases risk of nerve
involvement with pain down the arm) - Getting hit from behind (rear-impact collision)
- Previous neck pain or headaches
- Previous similar injury
- Being unaware of the impending impact
- Poor posture at the time of impact (head, neck, or chest bent forward)
- Poor position of the headrest or no headrest
- Crash speed under 10 mph
- Being in the front seat as opposed to sitting in the back seat of the car
- Collision with a vehicle larger than yours
- Being of slight build
- Wearing a seatbelt (a seat belt should always be worn, but at lower speeds, a lap and shoulder type seat belt will increase the chances of injury)

Symptoms
What are some of the symptoms of whiplash?
- Neck pain or neck pain that travels down the arm (radiculopathy)
- Headaches
- Low back pain (LBP)
- Jaw pain
- Dizziness
Ninety percent of patients involved in whiplash type accidents complain of neck pain. This is by far the most common symptom. The pain often spreads into the upper back, between the shoulder blades, or down the arm. Neck pain that goes down the arm is called radiculopathy.
Low back pain (LBP) can occur as a result of a whiplash injury. The Insurance Research Council reports that LBP occurs in 39 per cent of whiplash patients. Some studies found LBP to be present in 57 per cent of rear-impact collisions in which injuries were reported and 71 per cent of side-impact collisions.
Jaw pain as a result of temporomandibular joint (TMJ) injury can also cause painful headaches. The TMJ is formed by the bone of the mandible (lower jaw) connecting to the temporal bone at the side of the skull. The TMJ is a hinge joint that allows the jaw to open and close and to move forward, back, and sideways. Pain in this joint in called temporomandibular joint disorder (TMD).
Dizziness is quite common with a sense of lost balance being reported. It is caused by an injury to the joints of the neck called facet or zygapophyseal joints. When dizziness is reported, it should be distinguished from vertigo (also known as benign paroxysmal positional vertigo (BPPV), which results from an injury to the inner ear.
Other symptoms often reported include, but are not limited to: shoulder pain; numbness or tingling in the arms, hands, legs or feet; facial pain, fatigue, confusion, poor concentration, irritability, difficulty sleeping, forgetfulness, visual problems, and mood disorders.
It is not uncommon to have a delay in your symptoms. It is actually more common to have a 24 to 72 hour delay as opposed to immediate symptoms or pain. This is most likely due to the fact that it takes the body 24 to 72 hours to develop inflammation. Disc injuries may take even longer to manifest themselves. It is not uncommon for a disc injury to remain pain free and unnoticed for weeks to months.
Simply because there is little or no damage to your car does not mean that you were not injured. In fact, more than half of all whiplash injuries occur where there was little or no damage to one or both of the vehicles involved.
When we see visible damage to a car, it means that the car has absorbed much of that force and less force is transmitted to the occupant. On the other hand, if there is little or no damage to the car, the force is not absorbed but transferred to the driver or passengers, potentially resulting in greater injury.
Diagnosis
At Greater Pittsburgh Physical Therapy & Sports Medicine, diagnosis of your neck problem begins with a thorough history of your condition and the involved car accident. We may first ask you to fill out a questionnaire describing your neck problem. Your physical therapist will then ask you questions to find out when you first started having problems, what makes your symptoms better or worse, and how the symptoms affect your daily activity. The information that you provide us with will help guide the physical examination.
Your physical therapist will then physically examine the muscles and joints of your neck. It is important for us to see how your neck is aligned, how it moves, and exactly where it hurts.
We may do some simple tests to check the function of the nerves. These tests measure your arm and hand strength, check your reflexes, and help determine whether you have numbness in your arms, hands, or fingers.
Some patients may be referred to other healthcare providers, such as a doctor or chiropractor, for further diagnosis and treatment. Once your diagnostic examination is complete, the physical therapists at Greater Pittsburgh Physical Therapy & Sports Medicine have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Greater Pittsburgh Physical Therapy & Sports Medicine provides services for physical therapy in Pittsburgh.
Our Treatment
What treatment options are available?
Whenever possible, treatments other than surgery are preferable. The first goal of these nonsurgical treatments is to ease your pain and other symptoms.
At Greater Pittsburgh Physical Therapy & Sports Medicine, our physical therapists will work with you to improve your neck movement and strength. We will also encourage healthy body alignment and posture. Conservative care may include immobilization and other physical therapy applications. These steps are designed to enable you to get back to your normal activities.
Immobilization
At first, your physical therapist may prescribe immobilization of the neck. Keeping the neck still for a short time can calm inflammation and pain. This might include one to two days of bed rest and the use of a soft cervical (neck) collar.

The collar is a padded ring that wraps around the neck and is held in place by a Velcro strap. A soft cervical collar is generally used for the first 24 to 48 hours after neck injury to help provide support and reduce pain. There is usually no need for a hard or rigid cervical collar unless the neck is fractured.
Soft collars should not be worn for more than 48 hours without a health care provider’s approval. Studies show that prolonged immobilization can delay healing and promote disability. Wearing it longer tends to weaken the neck muscles and reduces the facet joints’ sense of position (proprioception).
Our physical therapist may also recommend a cervical support pillow for additional support while sleeping. This type of pillow helps to keep the neck in a more neutral position. Cervical pillows can be used any time by anyone for improved alignment while sleeping.
Our Physical therapy Program
Once you begin your physical therapy program at Greater Pittsburgh Physical Therapy & Sports Medicine, your rate of recovery helps determine the length of time you will be in physical therapy. Although recovery time is different for everyone, as a guideline, many whiplash patients only need to attend therapy sessions for two to four weeks. Patients with delayed recovery may need longer time in rehab.
When you first visit Greater Pittsburgh Physical Therapy & Sports Medicine, treatment is focused on easing pain and reducing inflammation. Our physical therapists may use ice and electrical stimulation treatments to help with these goals. Electrical stimulation treatments in addition to massage and other hands-on treatment can help calm muscle spasm and pain.
If your injury is deemed stable, we may also recommend traction. Traction is a way to gently stretch the joints and muscles of the neck. It can be done using a machine with a special head halter, or our therapist may apply the traction pull by hand. We may also add active treatments within the comfortable range of motion, and teach you specific exercises to help tone and control the muscles that stabilize your neck and upper back.
Our physical therapist will work with you on how to move and do activities. This form of treatment, called body mechanics, is used to help you develop new movement habits. Our training helps you keep your neck in safe positions as you go about your work and daily activities. We will help you learn how to keep your neck safe while you lift and carry items and as you begin to do other heavier activities.
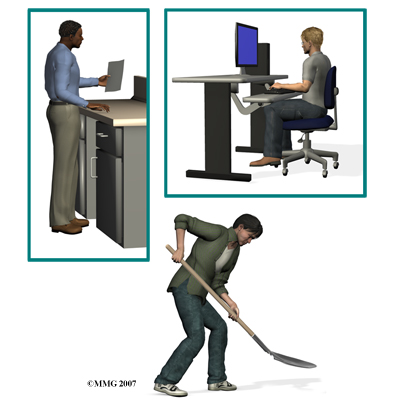
As your condition improves, our physical therapist will begin tailoring your program to help prepare you to go back to work. Some patients are not able to go back to a previous job that requires heavy and strenuous tasks. We may suggest changes in job tasks that enable you to go back to your previous job, or provide ideas for alternate forms of work. Our physical therapist will help you learn to do your tasks in ways that keep your neck safe and free of extra strain.
There is a strong emphasis on keeping as active as possible, which includes incorporating manual treatments and exercise. Before your Greater Pittsburgh Physical Therapy & Sports Medicine rehab program ends, we will teach you how to maintain any improvements you’ve made and ways to avoid future problems.
Although each individual heals at a different pace, you should expect full recovery to take up to three months. Rehabilitation and manipulative therapy is central in getting back to your pre-injury status.
At Greater Pittsburgh Physical Therapy & Sports Medicine, our goal is to help you keep your pain under control, improve your range of motion, and maximize strength and control in your neck. When your recovery is well under way, regular visits to our office will end. We will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Greater Pittsburgh Physical Therapy & Sports Medicine provides services for physical therapy in Pittsburgh.
Physician Review
How do doctors diagnose the problem?
There are several different types of test that you doctor may order to provide infomration on the extent of your whiplash injury.
Radiological Imaging
Radiological imaging tests help your doctor see the anatomy of your spine. There are many kinds of imaging tests including:
- X-rays
- Magnetic resonance imaging (MRI)
- Computed tomography (CT)
- Digital motion x-ray (DMX)
- Myelogram
- Bone Scan
- Electromyogram
X-rays show problems with bones, such as infection, bone tumors, or fractures. X-rays of the spine also can give your doctor information about how much degeneration has occurred in the spine, such as the amount of space in the neural foramina and between the discs.
X-rays are usually the first test ordered before any of the more specialized tests. Special x-rays called flexion/extension x-rays may help to determine if there is instability between vertebrae. These x-rays are taken from the side as you bend as far forward and then as far backward as you can. Comparing the two x-rays allows the doctor to see how much motion occurs between each spinal segment.
Magnetic resonance imaging (MRI)
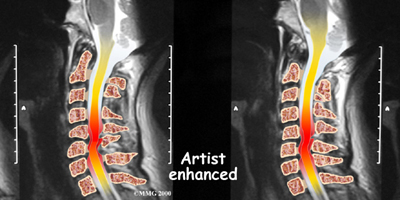
If more information is needed, your doctor may order an MRI. The MRI machine uses magnetic waves rather than x-rays to create pictures of the cervical spine in slices. MRIs show the cervical spine vertebrae, as well as the soft tissue structures, such as the discs, joints, and nerves. MRI scans are painless and don't require needles or dye. MRI scan has become the most common test to look at the cervical spine after x-rays have been taken.
Computed Tomography (CT)
CT scan is a special type of x-ray that lets doctors see slices of bone tissue. The machine uses a computer and x-rays to create these slices. It is used primarily when problems are suspected in the bones.
Digital motion x-ray (DMX)
DMX is a new fluoroscopic based x-ray system designed to objectively detect and document soft tissue/ligament injury most commonly associated with whiplash injuries of the spine. DMX evaluates biomechanical relationships and abnormal movements of the cervical spine. Specifically, DMX:
- Shows abnormal movement of vertebral bodies, facets, and other spinal elements
- Shows joint hypermobility, hypomobility, or restriction
- Shows normal or abnormal initiation of cervical motion
Example of DMX diagnostic video fluoroscopy.
DMX uses digital and optic technology now available. DMX is the latest generation of videofluoroscopy (VF) that uses low doses of radiation. The images have improved clarity and resolution over VF and are recorded digitally on CD or DVD disc. DMX digital images can be replayed and studied on standard computer systems. DMX images are simply x-ray images taken at 30 frames per second to form a multiple radiographic array or series that can be run as a movie file to display real time motion of the joints of the body.
DMX radiographic series can be paused at any location and the measurements and interpretation common to radiology can be applied to the still images. These images would be identical to plain film images if plain film radiography were performed at the same location at the same moment in motion. DMX acquires approximately 2700 images for the same amount of radiation as seven regular x-rays.
For more information visit http://www.dmxofmontana.com
Myelogram
The myelogram is a special kind of x-ray test where a special dye is injected into the spinal sac. The dye shows up on an x-ray. It helps a doctor see if there is a herniated disc, pressure on the spinal cord or spinal nerves, or a spinal tumor. Before the CT scan and the MRI scan were developed, the myelogram was the only test that surgeons had to look for a herniated disc. The myelogram is still used today but not nearly as often. The myelogram is usually combined with CT scan to give more detail.
Bone Scan
A bone scan is a special test where radioactive tracers are injected into your blood stream. The tracers then show up on special x-rays of your neck. The tracers build up in areas where bone is undergoing a rapid repair process, such as a healing fracture or the area surrounding an infection or tumor. Usually the bone scan is used to locate the problem and other tests such as the CT scan or MRI scan are then used to look at the area in detail.
Electromyogram (EMG)
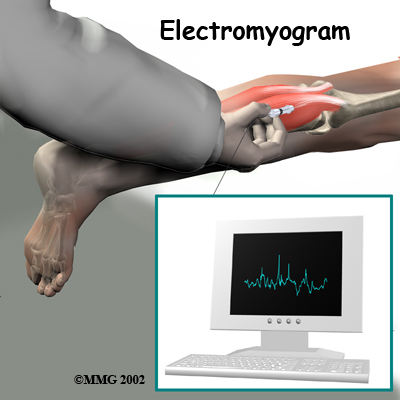
An electromyogram (EMG) is a special test used to determine if there are problems with any of the nerves going to the upper limbs. EMGs are usually done to see if one or more nerve roots have been pinched by a herniated disc. During the test, small needles are placed into certain muscles that are supplied by each nerve root. If there has been a change in the function of the nerve, the muscle will send off different types of electrical signals. The EMG test reads these signals and can help determine which nerve root is involved.
Grading the Severity of Injury
The physical exam combined with the imaging studies help determine the severity or grade of the injury. There is more than one way to assign a grade to a patient’s whiplash. Here are two examples of the more commonly used models used to classify or grade whiplash injuries:
Croft Guidelines
- Grade I: Minimal – No limitation of motion, no ligamentous injury, no neurological findings
- Grade II: Slight – Slight limitation of motion, no ligamentous injury, no neurologic findings
- Grade III: Moderate – Limitation of motion, ligamentous instability, neurologic symptoms present
- Grade IV: Moderate-to-Severe – Limitation of motion, some ligamentous injury, neurological symptoms, fracture or disc derangement
Quebec Whiplash Classification
- Grade 0: No complaint or physical sign
- Grade I: Neck complaint of pain, stiffness or tenderness, no physical signs
- Grade II: Neck pain and musculoskeletal signs
- Grade III: Neck pain and neurological signs
- Grade IV: Neck pain and fracture or dislocation
Medication
Your doctor may prescribe certain types of medication if the nerves are irritated or compressed and you have neck pain that travels down your arm (radiculopathy). Severe symptoms may be treated with narcotic drugs, such as codeine or morphine. But these drugs should only be used for the first few days or weeks after problems with radiculopathy start because they are addictive when used too much or improperly. Muscle relaxants may be prescribed to calm neck muscles that are in spasm. You may be prescribed anti-inflammatory medications such as aspirin or ibuprofen. Ensure that you consult with your doctor or pharmacist regarding the use of pain relief or anti-inflammatory medication.
Injection
Pain resulting from irritation of the facet joints may be alleviated with injection of an anesthetic agent similar to Novacaine such as Bipuvacaine. Your doctor may use this numbing agent to both confirm the source of pain as coming from the joint and help reduce or eliminate your pain.
