Introduction
Physical therapy in Pittsburgh for Ankle
Welcome to Greater Pittsburgh Physical Therapy & Sports Medicine's patient resource about Artificial Joint Replacement of the Ankle.
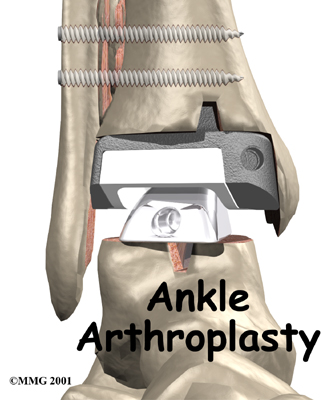
Surgery to replace the ankle joint with an artificial joint (called ankle arthroplasty) is becoming more common. This surgery is not done as often as replacement of the knee or hip joints. Still, when necessary, this operation can reduce the pain from arthritis of the ankle. Recent advances in the design of the artificial ankle and changes in the way the operation is performed have made artificial ankle replacement a growing alternative to ankle fusion for the treatment of ankle arthritis.
This guide will help you understand:
- why artificial ankle replacement becomes necessary
- what happens during surgery
- what to expect after treatment
Related Document: Greater Pittsburgh Physical Therapy & Sports Medicine's Guide to Osteoarthritis of the Ankle
Anatomy
How does the ankle joint work?
The ankle joint is made up of three bones: the lower end of the tibia (shinbone), the fibula (the small bone of the lower leg), and the talus, the bone that fits into the socket formed by the tibia and fibula. The talus sits on top of the calcaneus (the heelbone). The talus moves mainly in one direction. It works like a hinge to allow your foot to move up and down.
Ligaments on both sides of the ankle joint help hold the bones together. Many tendons cross the ankle to move the ankle and the toes. (Ligaments connect bone to bone, while tendons connect muscle to bone.) The large Achilles tendon at the back of the ankle is the most powerful tendon in the foot. It connects the calf muscles to the heelbone and gives the foot the power for walking, running, and jumping.
Inside the joint, the bones are covered with a slick material called articular cartilage. Articular cartilage is the material that allows the bones to move smoothly against one another in the joints of the body. The cartilage lining is about one-quarter of an inch thick in most joints that carry body weight, such as the ankle, hip, or knee. It is soft enough to allow for shock absorption but tough enough to last a lifetime, as long as it is not injured.
Related Document: Greater Pittsburgh Physical Therapy & Sports Medicine's Guide to Ankle Anatomy
Rationale
What does the surgeon hope to accomplish?
The symptoms of osteoarthritis of the ankle are pain and reduced movement in the ankle joint. The pain is typically aching in nature and can make walking difficult. Certain movements may cause a grinding or catching sensation as the arthritic bone surfaces move against one another. The ankle joint may swell. This swelling is worse after heavy use at first, but as the problem grows worse the ankle may stay swollen all the time. Bone spurs, or outgrowths, may form around the edges of the joint and can also be a source of pain and swelling. The benefit of an artificial joint is to ease the symptoms of ankle osteoarthritis and provide you with a mobile joint.
Preparation
The decision to proceed with surgery should be made jointly by you and your surgeon only after you feel that you understand as much about the procedure as possible.
Once the decision to proceed with surgery is made, several steps may be needed. Your orthopedic surgeon may suggest a complete physical examination by your medical or family doctor. This is to ensure that you are in the best possible condition to undergo the operation.
You may also need to spend time with the physical therapist who will be managing your rehabilitation after the surgery. One purpose of this preoperative visit is to record a baseline of information. This includes measurements of your current pain levels, functional abilities, and the available movement and strength of each ankle. A second purpose of the preoperative visit is to prepare you for your upcoming surgery. You'll begin to practice using crutches since you will need to use these for several weeks after surgery. Finally, an assessment will be made of any needs you'll have at home once you're released from the hospital.
On the day of your surgery, you will probably be admitted to the hospital early in the morning. You will be instructed to not eat or drink anything after midnight the night before surgery. You should plan on being in the hospital for several nights following surgery. The amount of time a patient spends in the hospital varies. You will need to stay until your medical condition has stabilized and you can safely use crutches or a walker.
The artificial ankle
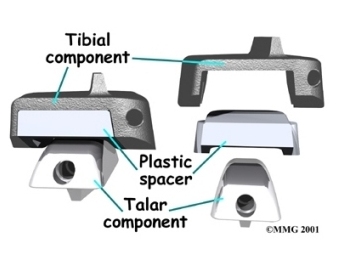
Each artificial ankle prosthesis is made of two parts:
- The tibial component is the part of the artificial joint that replaces the socket portion of the ankle (the top section).
- The talus component replaces the top of the talus.
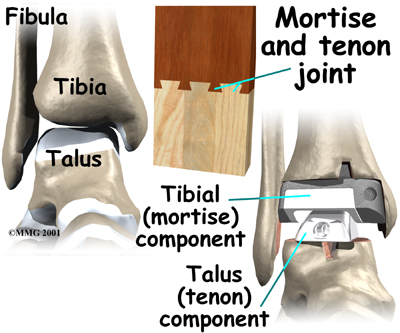
The tibial component is usually made up of two parts: a flat metal piece called a metal tray that is attached directly to the tibia bone, and a plastic cup that fits onto the metal piece, forming a socket for the artificial ankle joint. The talus component is made of metal and fits into the socket of the tibial component.
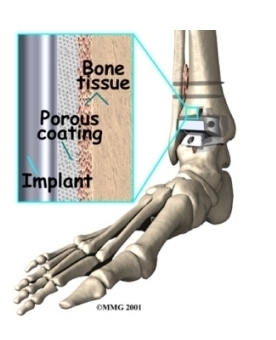
Your surgeon may use a special type of epoxy cement to attach the metal components to the bone. This is called a cemented prosthesis.
Cemented Prosthesis
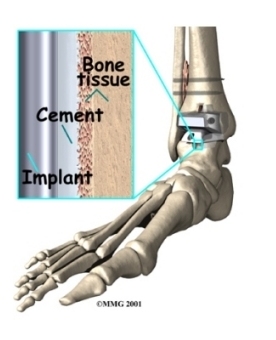
Some surgeons prefer to put the new joint in without using cement. This is called an uncemented prosthesis. The surface of this type of prosthesis bears a fine mesh of holes that allow bone to grow into the mesh and attach the prosthesis to the bone.
Uncemented Prosthesis
The Operation
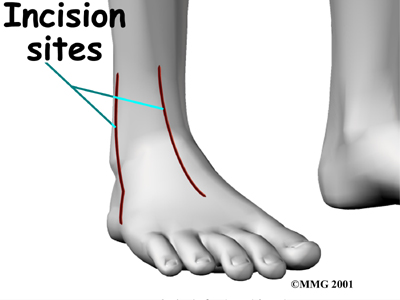
Before surgery you will be placed under either general anesthesia or a spinal type of anesthesia. The surgeon begins the operation by making an incision through the skin on the front of the ankle. Once through the skin, the nerves and blood vessels are protected and moved to the side. The tendons are also moved to the side. An incision is then made into the joint capsule that encloses the ankle joint. The surgeon opens the joint to prepare the surfaces to be replaced.
Incision
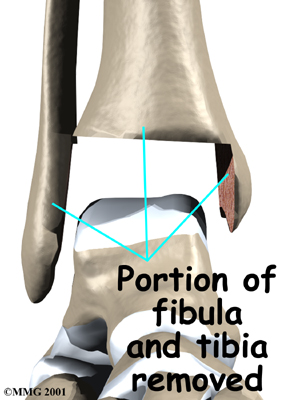
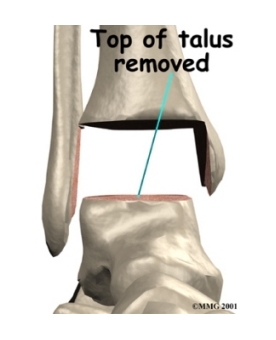
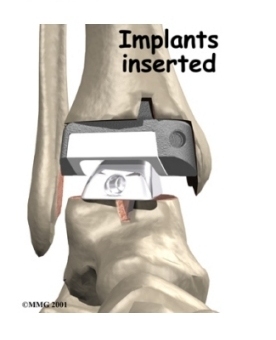
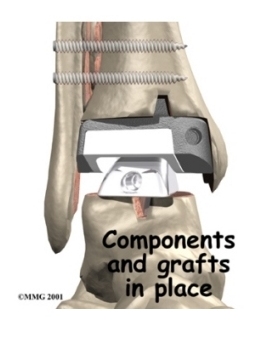
To fit the metal socket in place, the ends of the ankle bones are shaped. The tibia and fibula are shaped first. Next, the top of the talus is shaped so the metal talus component can be inserted. Finally, all the different pieces of the artificial ankle joint are put in place, and the ankle is tested to make sure the pieces fit properly.
Tibia and Fibula
Talus Shaped
Aritificial Ankle Joint Put in Place
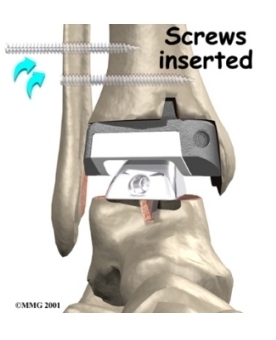
To make sure that the ankle socket or the tibial component fits tightly, two screws are placed through the fibula and the tibia just above the artificial ankle joint.
Screws Inserted
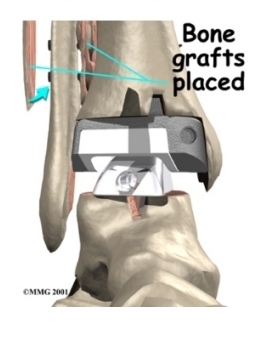
Bone is grafted between the fibula and tibia to create a fusion between them. This stops any motion between the two bones that could loosen the artificial joint. The bone graft is taken from the bone that was removed from the ankle earlier during the shaping procedure.
Bone Grafted
When the surgeon feels that everything is satisfactory, the joint capsule is sewn back together, and the skin is stitched together. A large bandage and splint are placed on the lower leg to protect the new ankle joint as your leg heals.
View animation of incision
View animation of tibial implant
View animation of talus implant
View animation of screw placement
View animation of insertion of bone graft material
Complications
As with all major surgical procedures, complications can occur. This document doesn't provide a complete list of the possible complications, but it does highlight some of the most common problems. Some of the most common complications following artificial ankle replacement are:
- anesthesia
- infection
- loosening
- nerve injury
Anesthesia
Problems can arise when the anesthesia given during surgery causes a reaction with other drugs the patient is taking. In rare cases, a patient may have problems with the anesthesia itself. In addition, anesthesia can affect lung function because the lungs don't expand as well while a person is under anesthesia. Be sure to discuss the risks and your concerns with your anesthesiologist.
Infection
Infection can be a very serious complication following an artificial joint surgery. The chance of getting an infection following artificial ankle replacement is probably two to four percent. This is somewhat higher than the risk of infection after a hip or knee replacement.
Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. Your surgeon may want to make sure that you take antibiotics when you have dental work or surgical procedures on your bladder or colon to reduce the risk of spreading germs to the joint.
Loosening
The major reason that artificial joints eventually fail continues to be a process of loosening of the metal or cement from the bone. Great advances have been made in extending how long an artificial joint will last, but most will eventually loosen and require a revision.
In the past, the artificial ankle has not been considered as successful as the hip and knee replacement. The artificial ankle replacement has a much higher risk of loosening and failure. Many have lasted only five to eight years. The risk of loosening is much higher in younger, more active patients and patients who are overweight. A loose prosthesis is a problem because it causes pain. Once the pain becomes unbearable, another operation will probably be required to either revise the ankle replacement or perform an ankle fusion.
Related Document: Greater Pittsburgh Physical Therapy & Sports Medicine's Guide to Ankle Fusion
Nerve Injury
All of the nerves and blood vessels that go to the foot travel across the ankle joint. Since the operation is performed so close to these important structures, it is possible to injure either the nerves or the blood vessels during surgery. The result may be temporary if the nerves have been stretched by retractors holding them out of the way. It is rare to have permanent injury to either the nerves or the blood vessels, but it is possible.
After Surgery
What happens after surgery?
Your ankle will probably be placed in a cast or splint after surgery. A small plastic tube may drain blood from the joint. Draining prevents excessive swelling from the blood. (This excess swelling is sometimes called a hematoma.) The draining tube will likely be removed within the first day.
Your surgeon will want to check your ankle within five to seven days. Stitches will be removed after 10 to 14 days, although most of them will have been absorbed into your body. You may have some discomfort after surgery. Your surgeon can give you medication to control any pain.
You should keep your ankle elevated above the level of your heart for several days to avoid swelling and throbbing. Keep it propped up on a stack of pillows when sleeping or sitting.
X-rays will be taken several times after your surgery to make sure that the artificial joint has not moved out of place and that the fusion between the fibula and the tibia is forming. When the uncemented type of implant is used, X-rays also help determine whether bone is attaching to the metal implant.
Our Rehabilitation
What should I expect during my recovery period?
For most patients who have undergone this procedure, the physical therapists at Greater Pittsburgh Physical Therapy & Sports Medicine will recommend that you use crutches or a walker for 10 to 12 weeks following surgery. During this time, you'll probably wear a cast or ankle splint and will be advised against putting weight on your foot when standing or walking.
Our physical therapists* at Greater Pittsburgh Physical Therapy & Sports Medicine will provide you with a personalized recovery program. Although the time required for recovery from ankle replacement surgery varies for each patients, as a guideline you may expect rehabilitation to take up to three months. When you begin rehab, our therapist will check to make sure you are using your walker or crutches safely and that you are placing only the prescribed amount of weight on your foot.
You first few physical therapy treatments at Greater Pittsburgh Physical Therapy & Sports Medicine will focus on controlling the pain and swelling from surgery. Our therapist may use heat treatments, gentle massage and other hands-on therapies to ease muscle spasm and pain.
Range-of-motion exercises are used to maximize the mobility of the new ankle joint, and strengthening exercises help improve stability around the joint. As with any surgery, you need to avoid doing too much, too quickly.
Our physical therapists sometimes design pool physical therapy programs for patients after artificial ankle joint surgery. Exercising in a swimming pool puts less stress on the new ankle joint, and the buoyancy lets you move and exercise easier. Once you've gotten your pool exercises down and the other parts of your Greater Pittsburgh Physical Therapy & Sports Medicine rehabilitation program advance, you may be instructed in an independent program.
Other exercises you'll do are designed to get your leg and ankle working in ways that are similar to your work tasks and daily activities. Our therapist will help you find ways to do your tasks that don't put too much stress on your ankle joint. Before your physical therapy sessions end, our physical therapist will teach you a number of ways to avoid future problems.
At Greater Pittsburgh Physical Therapy & Sports Medicine, our goal is to help you control your pain, improve your strength and range of motion, and walk smoothly and without a limp. When you are well under way, regular visits to our office will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Greater Pittsburgh Physical Therapy & Sports Medicine provides physical therapy in Pittsburgh.
Portions of this document copyright MMG, LLC.
